The Gut-Brain Reckoning: India is at a critical juncture in its public health journey. While conversations around mental health awareness have gained unprecedented traction, there remains a hidden factor threatening to undermine these strides: the rampant overuse of antibiotics. Traditionally, antibiotics have been hailed as miracle drugs, saving countless lives from infectious diseases. However, in India, where these medications are often consumed without prescriptions or proper medical oversight, their misuse has snowballed into a crisis that extends far beyond antimicrobial resistance.
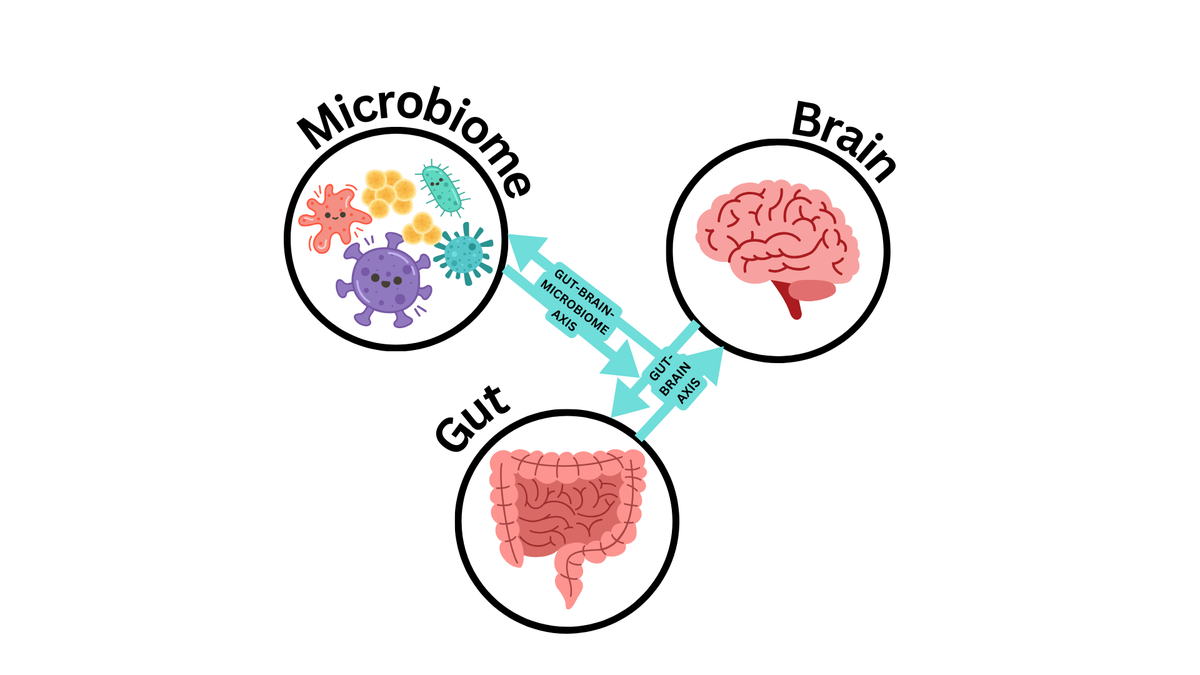
At the heart of this issue lies the gut-brain axis—a complex communication system linking the gut and the brain. Mounting scientific evidence shows that gut health plays a decisive role in regulating emotions, cognition, and psychological resilience. Antibiotics, by disrupting gut microbiota, can destabilize this axis and contribute to anxiety, depression, and cognitive decline. What was once considered solely a matter of infection control now emerges as a crucial determinant of mental well-being.
This intersection of gut health and mental health has profound implications for India. With mental health disorders already accounting for a significant portion of the country’s disease burden, unchecked antibiotic misuse could be silently intensifying the crisis. A deeper understanding of the gut-brain connection and responsible stewardship of antibiotics are essential if India hopes to safeguard both physical and psychological health in the decades to come.
The Gut-Brain Axis: A Hidden Highway of Communication
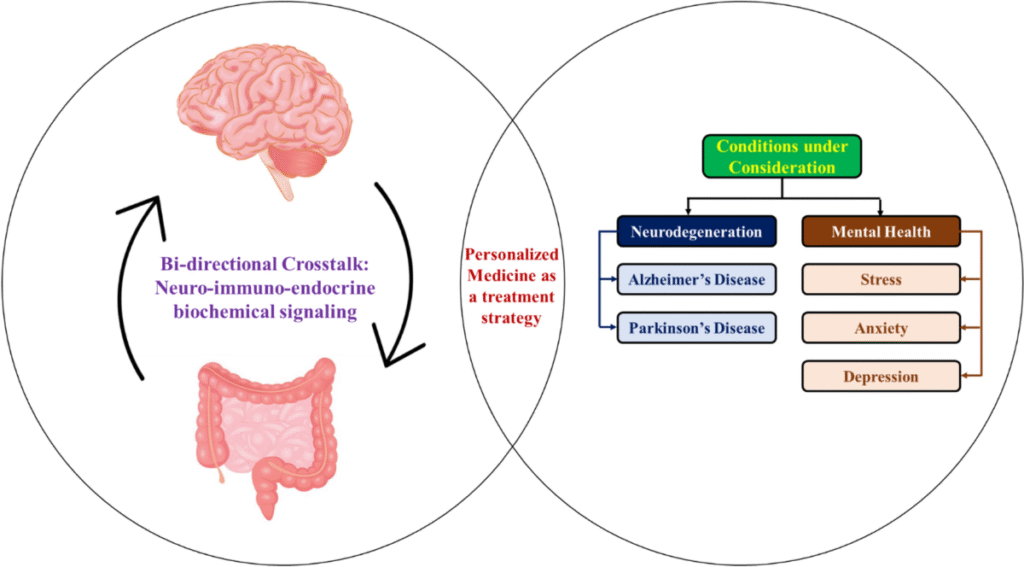
The gut-brain axis refers to the bidirectional communication network between the digestive system and the central nervous system. This relationship is mediated by the vagus nerve, immune pathways, and chemical messengers such as neurotransmitters. Gut microbes, in particular, play a central role in producing compounds like serotonin, dopamine, and gamma-aminobutyric acid (GABA), which influence mood and cognition.
Disruptions to this microbiome balance—often caused by antibiotics—can reduce the production of these crucial chemicals. The result is a higher susceptibility to mood disorders, stress intolerance, and cognitive impairment. For example, studies indicate that individuals with disturbed gut microbiota show greater risks of major depressive disorder (MDD) and generalized anxiety disorder (GAD).
Read about: How AI is Helping Healthcare Experts Deliver Smarter, More Timely Addiction Recovery Care
India’s Antibiotic Culture: Convenience Over Caution
India is one of the world’s largest consumers of antibiotics. Pharmacies frequently dispense them without prescriptions, and self-medication is rampant. Contributing factors include:
- Easy availability of antibiotics without regulation.
- Limited awareness about long-term side effects.
- Healthcare access disparities, where antibiotics are used as quick fixes instead of comprehensive care.
- Cultural reliance on fast relief, often prioritizing immediate symptom management over sustainable health practices.
This culture of casual antibiotic use not only accelerates antimicrobial resistance (AMR) but also profoundly impacts mental health outcomes through gut microbiome disruption.
Antibiotics and Mental Health: The Invisible Fallout
While AMR is widely acknowledged as a public health hazard, the mental health fallout of antibiotic misuse is often overlooked. Evidence suggests that frequent antibiotic exposure can:
- Lower microbial diversity, reducing resilience to stress.
- Increase risk of depression and anxiety disorders.
- Influence cognitive decline, potentially contributing to conditions like dementia.
- Affect sleep cycles and circadian rhythms by altering gut-brain chemical signaling.
This is particularly concerning in India, where mental health stigma often discourages people from seeking help, leaving many to silently bear the consequences of gut microbiota disruption.
Toward a Paradigm Shift: Integrating Gut Health into Mental Health Policies
India’s mental health discourse must expand to include microbial health. Policy interventions could include:
- Stricter regulation of antibiotic sales to curb misuse.
- Public health campaigns highlighting the connection between gut health and mental health.
- Encouraging probiotics and dietary diversity to restore microbial balance.
- Cross-disciplinary healthcare where psychiatrists, gastroenterologists, and primary care providers collaborate.
By shifting from a narrow view of antibiotics as infection-fighting drugs to a broader perspective of their systemic impacts, India can protect both its physical and mental health landscapes.
Also read: Amazon Launches Lens Live: Shop Instantly by Scanning Items with Your Camera
Conclusion
The gut-brain axis represents one of the most exciting frontiers in modern medicine, bridging microbiology, neurology, and psychiatry. In India, this axis is being undermined by the rampant, often unchecked, use of antibiotics. What begins as an attempt to cure infections may inadvertently erode emotional resilience and cognitive function, fueling a hidden mental health crisis.
Acknowledging the role of the microbiome in shaping psychological outcomes is essential. India cannot afford to compartmentalize physical and mental health when the two are deeply interconnected. By integrating gut health into mental health strategies, the nation can take a more holistic approach to wellness.
At the policy level, stronger regulations, public education, and medical accountability are urgently needed. Without these measures, the overuse of antibiotics will continue to chip away at both microbial diversity and collective well-being.
For individuals, awareness is the first line of defense. Mindful use of antibiotics, coupled with diets rich in fiber, fermented foods, and probiotics, can help restore balance and protect mental health. As India advances in mental health awareness, embracing the gut-brain reckoning is not just advisable—it is indispensable.
FAQs Of The Gut-Brain Reckoning
1. What is the gut-brain axis and why is it important?
The gut-brain axis is a communication system between the gastrointestinal tract and the brain, involving nerves, hormones, and gut microbes. It regulates mood, cognition, and emotional resilience. Disruption in this system, often caused by antibiotics, can increase risks of depression, anxiety, and memory decline.
2. How does antibiotic misuse affect mental health?
Antibiotics kill harmful bacteria but also disrupt beneficial gut microbes. This imbalance can impair the production of neurotransmitters like serotonin and dopamine, which are critical for mental well-being. Long-term misuse raises the risk of mood disorders and cognitive decline.
3. Why is antibiotic overuse such a problem in India?
Antibiotics are easily available over the counter in India, and many people self-medicate without medical guidance. Lack of regulation, limited healthcare access, and cultural habits of seeking fast relief contribute to excessive use.
4. Can diet and probiotics help restore gut health after antibiotic use?
Yes. A diet rich in prebiotics (fiber) and probiotics (fermented foods like yogurt, kefir, and pickles) can help restore microbial diversity. These foods support gut health and may improve mental resilience by rebalancing the gut-brain axis.
5. What steps should India take to protect mental health from antibiotic misuse?
Key steps include enforcing stricter regulations on antibiotic sales, educating the public about long-term risks, integrating gut health into mental health policies, and encouraging cross-disciplinary medical care. These measures can reduce both antimicrobial resistance and mental health risks.