Does Your LDL or Bad Cholesterol: Can the calcium supplement you take for stronger bones also support your heart by lowering your bad cholesterol levels? The relationship between calcium and cardiovascular health has been a subject of growing scientific interest. Traditionally, calcium supplements are known for maintaining bone density and preventing osteoporosis. However, emerging evidence suggests that they may also play a modest role in managing low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol, which is linked to an increased risk of heart disease.
Over the past few years, numerous clinical trials and meta-analyses have examined calcium’s influence on serum lipids and cholesterol levels. While the findings are mixed, a recurring pattern is beginning to emerge: calcium may help lower LDL cholesterol in certain individuals, particularly when combined with other healthy lifestyle habits. However, experts emphasize that calcium’s effect on cholesterol is not universal or strong enough to replace established treatment methods like diet, exercise, or prescribed medications.
According to Dr. Rakesh Gupta, Senior Consultant, Internal Medicine at Indraprastha Apollo Hospitals, New Delhi, “Calcium’s impact on cholesterol depends on dosage, duration, and an individual’s metabolic profile. It is not a one-size-fits-all solution.” Understanding how calcium interacts with fats in the body helps shed light on this complex connection — one that intertwines bone health with heart wellness.
How Calcium Supplementation Might Affect Cholesterol
When calcium is consumed as a supplement, it influences how the body absorbs and processes fats and cholesterol. One key mechanism is its ability to bind with fatty acids and bile acids in the intestine. This process forms insoluble compounds that prevent fats and cholesterol from being absorbed into the bloodstream. Instead, these compounds are excreted from the body, leading to a potential reduction in circulating cholesterol levels.
Additionally, calcium may affect lipid metabolism by altering the activity of certain enzymes involved in cholesterol synthesis and breakdown. Over time, this interaction can improve lipid profiles, particularly in people who are not already on cholesterol-lowering medications.
Read about: TOI Medithon 2025: Expert Insights on Heart Health Across Generations
Research Findings on Calcium and Cholesterol
Several studies have explored calcium’s effect on cholesterol levels, and while outcomes vary, the general consensus suggests modest benefits:
- LDL Cholesterol Reduction:
Research shows that taking calcium supplements — particularly doses of 1,000 mg or more daily for over 12 weeks — can result in a small but meaningful decrease in LDL cholesterol.
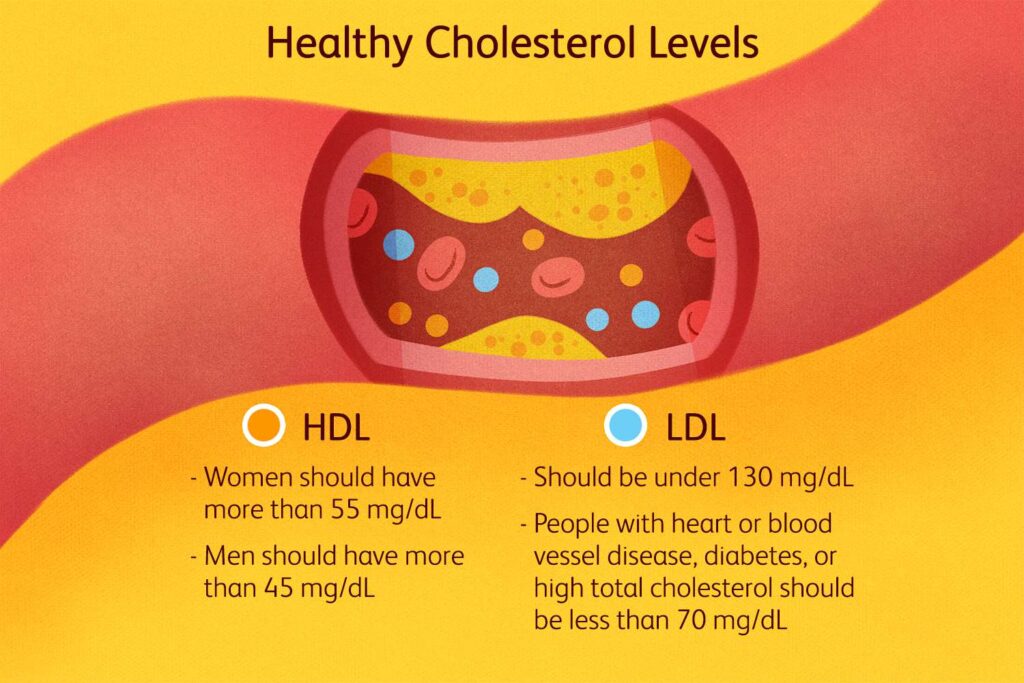
A 2023 meta-analysis found that calcium supplementation significantly reduced LDL levels in individuals without pre-existing lipid disorders. - Impact on HDL (Good Cholesterol):
The effect of calcium on HDL cholesterol is less consistent. Some studies report a slight increase in HDL and improvements in the HDL/LDL ratio, indicating better overall lipid balance. - Triglyceride Reduction:
Clinical trials have found that calcium supplements can lower triglycerides by up to 30% when taken in higher doses (around 2 grams of elemental calcium daily for six months). - Total Cholesterol:
Changes in total cholesterol are generally modest — about a 5–7% decrease in some cases — though other studies find no significant change.
Overall, calcium supplementation appears to provide a secondary benefit for lipid management, especially in individuals not receiving other lipid-lowering therapies.
Population Differences and Potential Risks
The effect of calcium supplementation can vary significantly among populations, especially in postmenopausal women and high-risk individuals.
- Postmenopausal Women:
Some studies suggest that postmenopausal women with low estrogen levels may experience elevated cholesterol or triglycerides with high calcium intake. This may be due to hormonal changes that affect lipid metabolism. - Men and High-Risk Groups:
In certain men and individuals with existing cardiovascular disease, high calcium intake could theoretically contribute to arterial plaque formation, although large-scale studies have not conclusively proven this risk. - Heart Disease Controversy:
Concerns have been raised about whether calcium supplements might increase the risk of arterial calcification. However, most large meta-analyses have not found a clear link between calcium supplementation and increased heart attack or stroke risk.
Experts emphasize that the source of calcium matters — dietary calcium from food sources appears safer and more beneficial than excessive reliance on supplements.
Calcium is Best for Bone Health — Cholesterol Needs Separate Management
While calcium supplements may offer a modest cholesterol-lowering effect, they should not be used as a primary treatment for high LDL or total cholesterol. Their primary role remains in bone health, particularly for preventing osteoporosis in postmenopausal women and older adults.
For people already taking cholesterol-lowering medications such as statins, adding calcium supplements is unlikely to provide additional lipid benefits. Instead, calcium should be used to meet nutritional needs — ideally through food sources such as dairy products, leafy greens, sesame seeds, and fortified foods.
Ultimately, cholesterol management requires a multifaceted approach — combining balanced nutrition, regular exercise, stress management, and medical supervision when necessary.
Conclusion
The relationship between calcium supplements and cholesterol levels highlights how intricately connected our body systems are. While calcium’s primary function is to strengthen bones and maintain nerve and muscle function, it may also play a supportive role in improving lipid balance, particularly by reducing LDL and triglycerides in some individuals.
However, these benefits are modest and variable, depending on individual health profiles, dosage, and duration. Calcium supplementation should therefore be considered a complementary measure, not a substitute for proven cholesterol management strategies.
For optimal results, individuals should focus on dietary sources of calcium, such as milk, yogurt, tofu, and ragi, rather than excessive supplementation. Regular exercise, avoiding trans fats, and increasing fiber intake remain the cornerstone of cardiovascular health.
In conclusion, while calcium can offer a mild lipid-lowering benefit, the best way to protect both your bones and your heart is through a balanced lifestyle — one that integrates mindful nutrition, regular activity, and medical guidance tailored to your individual needs.
Also read: Senate Finance Committee Clears Donald Korb as IRS Chief Counsel Nominee
FAQs
1. Can calcium supplements really lower bad cholesterol (LDL)?
Yes, some studies have shown that calcium supplements may modestly lower LDL cholesterol, particularly when taken in doses of around 1,000 mg or more daily over 12 weeks or longer. However, the effect is small and varies between individuals.
2. How does calcium help reduce cholesterol levels?
Calcium binds to fatty acids and bile acids in the intestine, preventing the absorption of cholesterol into the bloodstream. This process leads to the excretion of cholesterol through the digestive tract, potentially reducing LDL levels.
3. Are calcium supplements safe for people with heart disease?
Most studies suggest that calcium supplements are safe when taken within recommended doses (up to 1,000–1,200 mg per day). However, people with heart disease or a history of kidney stones should consult their doctor, as excessive calcium may pose risks.
4. Should I take calcium supplements to control cholesterol?
No, calcium should not be taken solely to manage cholesterol. It can be a helpful secondary support but should primarily be used for maintaining bone health. For cholesterol control, focus on a heart-healthy diet, regular exercise, and medications if prescribed.
5. What’s the best source of calcium for overall health?
Natural dietary sources such as milk, yogurt, cheese, almonds, tofu, sesame seeds, and green leafy vegetables are preferred. They provide calcium along with other nutrients without the potential risks linked to high-dose supplementation.
