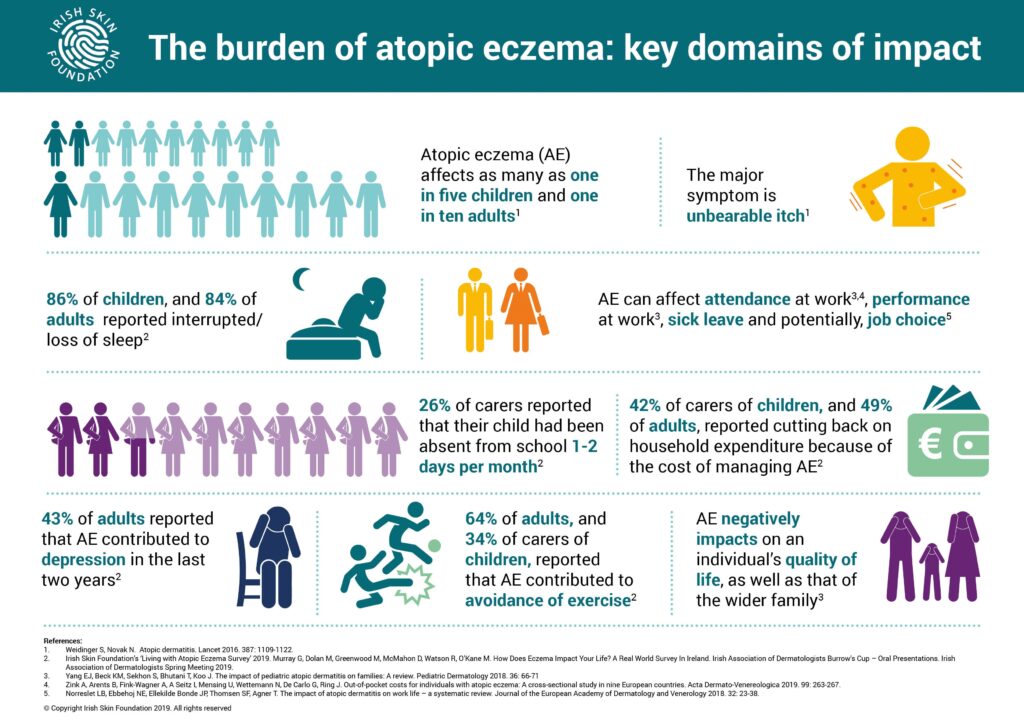
The Mental Health Burden of Atopic Dermatitis: Atopic dermatitis, the most common form of eczema, is often thought of as “just a skin condition,” but for millions of people, its impact reaches far deeper. Affecting up to 25% of children and 10% of adults worldwide, this chronic inflammatory disorder brings more than rashes and relentless itch—it introduces daily struggles with self-confidence, social interactions, and overall emotional well-being. Patients often describe sleepless nights, constant discomfort, and embarrassment from flare-ups that can appear anywhere on the body. These physical symptoms alone can leave a profound psychological mark.
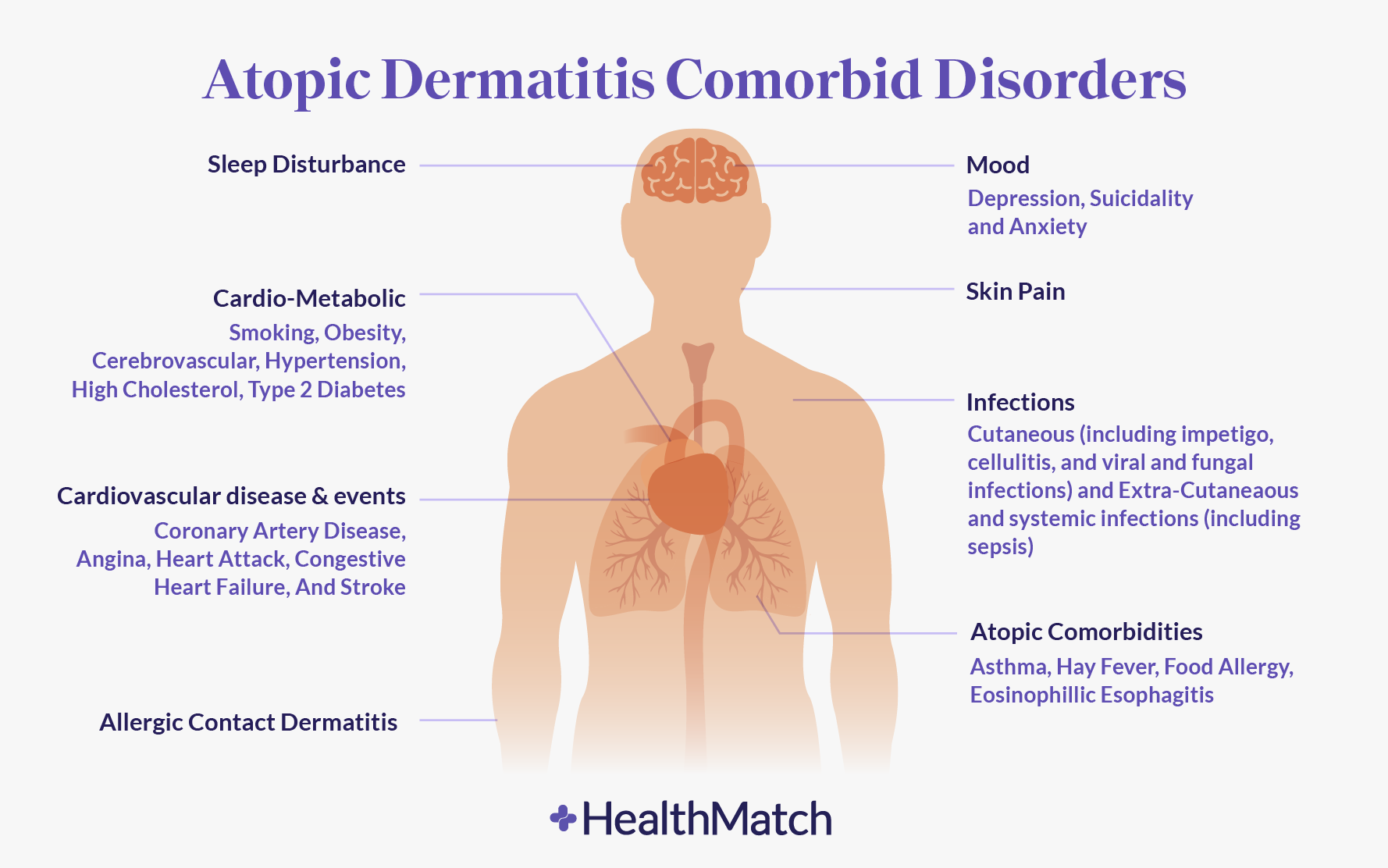
Increasingly, researchers and clinicians are recognizing that atopic dermatitis is not only a dermatological disease but also a mental health challenge. Studies over the past two decades consistently show associations between atopic dermatitis and neuropsychiatric conditions such as anxiety, depression, ADHD, OCD, cognitive and behavioral changes, and alexithymia (difficulty recognizing and expressing emotions). Adults with atopic dermatitis are estimated to have a 14–20% higher risk of depression compared to those without the condition. These statistics reflect not just coincidence but a pattern that highlights the skin-brain connection.
The burden of atopic dermatitis extends beyond visible lesions. For many patients, the relentless itch creates chronic sleep disturbances, which in turn fuel mental health challenges. Others experience social withdrawal due to embarrassment or stigma, which can lead to isolation and depression. With growing evidence of biological links such as neuroinflammation and genetic risk factors, scientists are now exploring whether the disease’s underlying mechanisms might directly contribute to neuropsychiatric conditions. This dual impact—both visible and invisible—has placed atopic dermatitis at the center of a much larger health conversation.
Understanding the Link Between Atopic Dermatitis and Mental Health
Psychological Strain of a Visible Disease
A visible condition like atopic dermatitis can erode self-esteem. Flare-ups on the face, hands, or arms make many patients feel self-conscious in public, avoiding social gatherings or relationships. This avoidance can lead to loneliness, anxiety, and depression, creating a cycle where mental health symptoms worsen physical ones.
Biological Pathways: More Than Skin Deep
Researchers believe there may be more than psychological factors at play. Inflammatory pathways, sleep disruption, and neuroimmune activity might contribute directly to psychiatric conditions. This raises the possibility that atopic dermatitis and certain mental health disorders share biological mechanisms, especially since both involve immune system dysfunction and chronic inflammation.
Read about: The Mental Health Burden of Atopic Dermatitis
Role of Sleep in Worsening Neuropsychiatric Outcomes
Sleep Disruption as a Mediator
One of the strongest connections between atopic dermatitis and mental health is poor sleep quality. Studies show that individuals with atopic dermatitis are two to four times more likely to experience sleep disorders such as insomnia or sleep apnea. The itch-scratch cycle often prevents children and adults alike from falling or staying asleep.
Consequences of Poor Sleep
Sleep deprivation is a well-established risk factor for anxiety, depression, impulsivity, and ADHD-like symptoms. In children, poor sleep can lead to irritability, attention difficulties, and reduced cognitive performance. Long-term, it can increase the risk of developmental and psychiatric diagnoses. One study found that children with atopic dermatitis who slept fewer than four nights per week adequately were two to five times more likely to receive an ADHD diagnosis.
Can Effective Treatment Improve Mental Health?
Dupilumab and Emerging Therapies
The introduction of advanced therapies like dupilumab, a monoclonal antibody that targets interleukin-4 (IL-4), has provided new hope. Clinical and retrospective studies show that patients treated with dupilumab experience improvements not only in their skin condition but also in anxiety, depression, sleep quality, and overall quality of life.
Preventing Mental Health Disorders
Recent research suggests that effective treatments may do more than relieve symptoms—they could reduce the risk of developing psychiatric conditions altogether. For example, a three-year retrospective study found that people on dupilumab were 24% less likely to develop anxiety and 30% less likely to develop depression compared to those using conventional therapies. Similarly, children treated with dupilumab were found to be 44% less likely to acquire a psychiatric diagnosis over two years.
Also read: Suzuki e-Access Price Reveal Soon – 95km Range, Rival to iQube & Rizta
Untangling Cause and Effect
Despite growing evidence, it remains difficult to determine whether atopic dermatitis causes mental health issues or simply shares overlapping risk factors with them. Social isolation, poor sleep, and inflammatory processes all contribute, but the precise mechanisms are still unclear. Large-scale, long-term studies such as the PEDISTAD international study, which follows children with moderate-to-severe atopic dermatitis over ten years, aim to shed light on whether early treatment can prevent later psychiatric diagnoses.
Conclusion
Atopic dermatitis is far more than a chronic skin condition—it is a disorder with far-reaching consequences for mental and emotional health. The daily challenges of persistent itching, disrupted sleep, and visible rashes weigh heavily on patients, often leading to anxiety, depression, or behavioral issues. For many, the emotional toll of the disease can feel just as devastating as the physical symptoms.
Research over the past two decades has made it clear that there is a strong connection between atopic dermatitis and mental health outcomes. Whether this link is primarily driven by inflammation, sleep disruption, or genetic predisposition remains an open question. However, what is certain is that mental health should be considered a core component of eczema care.
The arrival of advanced biologic therapies like dupilumab is transforming treatment possibilities. Not only do these drugs provide significant skin relief, but they also show promise in reducing psychiatric risks, improving quality of life, and potentially preventing mental health conditions before they emerge. This marks a significant step forward for patients who have long felt the dual burden of skin and psychological distress.
Ultimately, tackling the mental health burden of atopic dermatitis requires a holistic approach—one that combines medical treatment with psychological support, patient education, and early intervention. As researchers continue to untangle the complex relationship between skin and brain, the future of care looks brighter for the millions affected by this challenging condition.
FAQs About Atopic Dermatitis and Mental Health
1. Why does atopic dermatitis affect mental health?
Atopic dermatitis affects mental health through both psychological and biological pathways. The visible nature of the disease can reduce confidence, while constant itching disrupts sleep and daily life. Biologically, inflammation and immune dysregulation may also influence brain function, contributing to anxiety, depression, or ADHD-like symptoms.
2. What mental health conditions are most common in people with atopic dermatitis?
The most common conditions include anxiety and depression, but studies also show higher risks of ADHD, OCD, cognitive and behavioral changes, and alexithymia. Children with severe eczema are especially vulnerable to developmental and attention-related diagnoses.
3. Can treatment for atopic dermatitis improve mental health symptoms?
Yes. Effective treatments such as dupilumab not only reduce eczema symptoms but also improve mental health outcomes. Research shows that when atopic dermatitis is under control, patients report reduced anxiety, better sleep, and fewer depressive symptoms.
4. Is poor sleep the main reason eczema patients develop mental health problems?
Sleep plays a major role but is not the only factor. People with atopic dermatitis are more prone to sleep disturbances, which worsen anxiety, depression, and ADHD-like behaviors. However, researchers also believe that inflammation and genetic risk factors contribute to psychiatric risks independent of sleep.
5. Can early intervention in children reduce the risk of later mental health issues?
Emerging evidence suggests yes. Studies show that children treated with dupilumab or other advanced therapies are significantly less likely to develop psychiatric conditions later. Long-term studies like PEDISTAD are now underway to test whether early intervention can prevent mental health burdens across childhood and adolescence.











2 thoughts on “The Mental Health Burden of Atopic Dermatitis: Why the Skin-Brain Connection Matters”