Vaccines for Dementia: Dementia is one of the most pressing public health challenges of the 21st century — and one that continues to grow at an alarming rate. Globally, more than 55 million people are living with dementia, and nearly 10 million new cases are diagnosed each year. By 2050, experts estimate that this number will triple, creating an enormous burden on healthcare systems, caregivers, and families worldwide.
Dementia isn’t a single disease but an umbrella term for a range of neurological conditions that affect the brain’s structure and function. It leads to progressive declines in memory, cognition, mood, behavior, and personality. The most common forms include:
- Alzheimer’s disease – accounts for 60–70% of all dementia cases.
- Vascular dementia – caused by reduced blood flow to the brain.
- Dementia with Lewy bodies (DLB) – involves abnormal protein deposits that disrupt brain function.
- Frontotemporal dementia (FTD) – affects the brain’s frontal and temporal lobes.
Despite decades of research, there is no cure for dementia. Treatments available today can only manage symptoms or slow progression, but they do not stop the underlying disease process. This is why prevention strategies — including lifestyle changes, diet, exercise, and managing risk factors — are increasingly being emphasized by neurologists and public health experts.
1. Influenza (Flu) Vaccine: Annual Shots Linked to Lower Dementia Risk
The influenza vaccine — one of the most widely used vaccines in the world — is designed to protect against seasonal flu viruses. But new evidence suggests that it may offer long-term benefits far beyond flu prevention.
What the Research Says
A landmark study published in the journal Alzheimer’s & Dementia found that people who received at least one flu vaccine had a 40% lower risk of developing Alzheimer’s disease over the next four years compared to those who were not vaccinated. Moreover, individuals who received regular annual flu shots showed the greatest risk reduction.
Another large-scale study from Texas Health Science Center analyzed medical records of over 2 million adults aged 65+ and found similar results — flu vaccination was consistently associated with significantly reduced dementia incidence.
Why It May Work
Researchers believe the flu vaccine’s benefits may stem from its ability to reduce chronic inflammation — a key factor in Alzheimer’s and other dementias. Vaccines also train the immune system to respond more effectively, potentially preventing harmful inflammatory cascades in the brain triggered by infections.
Additionally, repeated vaccinations may stimulate immune memory, which improves the body’s overall defense mechanisms, including those that protect brain cells from neurodegeneration.
Who Should Get It
- Adults aged 50+ should receive an annual flu shot.
- High-risk groups (e.g., those with heart disease, diabetes, or compromised immunity) should not skip it.
- Even younger adults may benefit if they have a family history of dementia.
2. Pneumococcal Vaccine: Protecting Against Brain-Damaging Infections
The pneumococcal vaccine, which protects against Streptococcus pneumoniae infections such as pneumonia, meningitis, and sepsis, has also been linked to lower dementia risk.
What the Research Says
A 2020 study published in the journal Vaccine followed more than 5,000 adults aged 65+ and discovered that those who received the pneumococcal vaccine between ages 65 and 75 had a 25–30% lower risk of Alzheimer’s disease compared to those who did not.
Another analysis from the University of Texas showed that when the pneumococcal vaccine was combined with the flu vaccine, the dementia risk reduction was even greater — up to 40%.
Why It May Work
Pneumococcal infections are known to cause severe inflammation in the brain and central nervous system. Repeated infections — even mild ones — can accelerate cognitive decline and damage the blood-brain barrier, a crucial defense system that keeps harmful substances out of the brain.
By preventing such infections, the vaccine lowers the risk of inflammatory damage that could lead to dementia. Furthermore, some scientists suggest that pneumococcal vaccination might enhance brain resilience by modulating immune system responses.
Who Should Get It
- All adults aged 65+ are recommended to receive a pneumococcal vaccine.
- People with chronic conditions like diabetes, COPD, or cardiovascular disease should consider vaccination earlier, starting at age 50 or as advised by a doctor.
3. Tdap Vaccine (Tetanus, Diphtheria, Pertussis): Unexpected Protection for the Brain
The Tdap vaccine, typically given in childhood and boosted in adulthood, protects against tetanus, diphtheria, and pertussis (whooping cough). Surprisingly, research now suggests that it might also play a role in reducing dementia risk.
What the Research Says
A large cohort study by Stanford University School of Medicine found that adults who received the Tdap booster had a 30–35% lower risk of dementia compared to those who had not. The protective association remained strong even after adjusting for lifestyle factors, socioeconomic status, and preexisting conditions.
Interestingly, the benefit was most pronounced in people who received multiple boosters over their lifetime, suggesting a cumulative protective effect.
Why It May Work
The mechanism behind Tdap’s neuroprotective effect is still being studied, but experts believe it’s linked to immune system modulation. Chronic low-grade inflammation plays a key role in neurodegenerative diseases, and vaccines like Tdap help balance immune responses, preventing harmful inflammation that can damage neurons.
Additionally, preventing diseases like pertussis and diphtheria — both of which can lead to severe neurological complications — indirectly protects brain health in the long term.
Who Should Get It
- Adults should receive a Tdap booster every 10 years.
- Pregnant women are also advised to get a Tdap shot to protect both themselves and their newborns.
- Anyone with unknown vaccination history should discuss booster options with a healthcare provider.
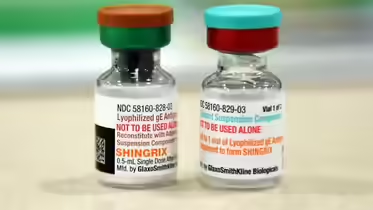
4. Shingles (Herpes Zoster) Vaccine: Guarding Against Cognitive Decline
The shingles vaccine is primarily recommended for older adults to prevent herpes zoster, a painful condition caused by the reactivation of the varicella-zoster virus (the same virus that causes chickenpox). However, emerging evidence suggests that it may also protect the brain from dementia.
What the Research Says
A 2023 study published in Neurology followed more than 200,000 older adults and found that those who received the shingles vaccine were 20–25% less likely to develop dementia over a 10-year period compared to unvaccinated individuals.
Similar findings from NIHR and Oxford University showed that the shingles vaccine could significantly delay the onset of cognitive decline, particularly in those aged 70 and older.
Why It May Work
Chronic viral infections, including herpes viruses, have long been suspected of contributing to Alzheimer’s disease and other dementias. These viruses can remain dormant in the body and reactivate periodically, triggering neuroinflammation that damages brain cells.
By preventing shingles reactivation, the vaccine reduces the risk of neuroinflammation and protects the brain from repeated immune system assaults. Additionally, preventing shingles-associated complications such as encephalitis may further reduce dementia risk.
Who Should Get It
- Adults aged 50 and above should receive the shingles vaccine.
- A two-dose series (usually spaced 2–6 months apart) is recommended for long-term protection.
- Even if you’ve had shingles before, vaccination is still advised to prevent recurrence.
Why Vaccines Might Protect Against Dementia
The idea that vaccines could lower dementia risk may seem surprising, but scientists believe several mechanisms could explain their protective effects:
- Reduced Neuroinflammation: Many infections trigger chronic inflammation, which can damage neurons and accelerate cognitive decline. Vaccines help prevent these infections and reduce long-term inflammation.
- Immune System Modulation: Vaccines “train” the immune system to respond more efficiently, which may enhance its ability to clear harmful proteins like beta-amyloid and tau, both linked to Alzheimer’s.
- Lower Infection Burden: Frequent infections — even if mild — increase dementia risk. By lowering the total burden of infections over a lifetime, vaccines indirectly protect the brain.
- Improved Vascular Health: Some infections can damage blood vessels and contribute to vascular dementia. Preventing them helps maintain healthy cerebral circulation.
The Bottom Line: Vaccination Is Brain Protection
While there’s still no cure for dementia, growing evidence suggests that vaccines — from flu shots to shingles boosters — can play a surprising and powerful role in lowering the risk of this devastating condition.
They’re not a silver bullet, but they can be a crucial part of a multi-pronged prevention strategy that includes:
- Regular physical activity
- A balanced, brain-healthy diet
- Good sleep hygiene
- Cognitive stimulation (reading, puzzles, social engagement)
- Management of blood pressure, cholesterol, and blood sugar
As scientists continue to explore the immune system’s role in brain health, vaccines could become an essential tool in the fight against dementia — offering hope for millions worldwide.
Takeaways
- Flu, pneumococcal, Tdap, and shingles vaccines are linked to a 20–40% reduced risk of dementia.
- Benefits likely stem from lower infection-related inflammation and immune system modulation.
- Regular vaccination, particularly in adulthood and older age, can delay or prevent cognitive decline.
- Vaccination should be part of a holistic brain health strategy that includes lifestyle and medical care.
FAQs
Q1: Can vaccines cure dementia?
No, vaccines cannot cure dementia. However, research suggests they can lower the risk or delay onset by reducing neuroinflammation and preventing brain-damaging infections.
Q2: Should younger adults get these vaccines too?
While the dementia risk is higher in older adults, starting preventive strategies earlier — including vaccination — can provide long-term benefits, especially for those with a family history of dementia.
Q3: Are there risks associated with these vaccines?
All vaccines have potential side effects (like mild fever or soreness), but serious reactions are rare. For most people, the benefits far outweigh the risks.
Q4: Will more dementia-specific vaccines become available in the future?
Scientists are actively developing vaccines that target amyloid plaques and tau proteins directly. While still in clinical trials, these may eventually complement existing vaccines in dementia prevention.
